What is a “Medicare Risk Adjustment Factor (RAF)?”
The purpose for the Centers for Medicare and Medicaid Services (CMS) to conduct Risk Adjustment Factors is to pay plans for the risk of the beneficiaries they enroll, instead of calculating an average amount of Medicare/Medicare Advantage beneficiaries. By doing so, CMS is able to make appropriate and accurate payments for enrollees with differences in expected costs. Lastly, the risk adjustment allows CMS to use standardized bids as base payments to plans.
CMS risk adjusts certain plan payments, such as Part C payments made to Medicare Advantage (MA) plans and Program for All Inclusive Care for The Elderly (PACE) organizations, and Part D payments made to Part D sponsors, including Medicare Advantage-Prescription Drug plans (MA-PDs) and standalone Prescription Drug Plans (PDPs).
Below is a high-level checklist of plan requirements with detailed information regarding risk adjustment data collection, submission, reporting, and validation:
- “Ensure the accuracy and integrity of risk adjustment data submitted to CMS. All diagnosis codes submitted must be documented in the medical record and must be documented as a result of a face-to-face visit.
- Implement procedures to ensure that diagnoses are from acceptable data source. The only acceptable data sources are hospital inpatient facilities, hospital outpatient facilities, and physicians.
- Submit the required data elements from acceptable data sources according to the coding guidelines.
- Submit all required diagnoses codes for each beneficiary and submit unique diagnoses once during the risk adjustment data-reporting period. Submitters must filter diagnosis data to eliminate the submission of duplicate diagnosis clutters.
- The plan sponsor determines that any diagnosis codes have been erroneously submitted, the plan sponsor is responsible for deleting the submitted diagnosis codes as soon as possible.
- Receive and reconcile CMS Risk Adjustment Reports in a timely manner. Plan sponsors must track their submission and deletion of diagnosis codes on an ongoing basis.
- Once CMS calculates the final risk scores for a payment year, plan sponsors can only request a recalculation of payment upon discovering the submission of erroneous diagnosis codes that CMS used to calculate a final risk score for a previous payment year and that had a material impact on the final payment. Plan sponsors must inform CMS immediately upon such a finding.”
Reference:
http://www.hfni.com/assets/forms/Medicare%20Managed%20Care%20Manual%20%28Risk%20Adjustment%29.pdf
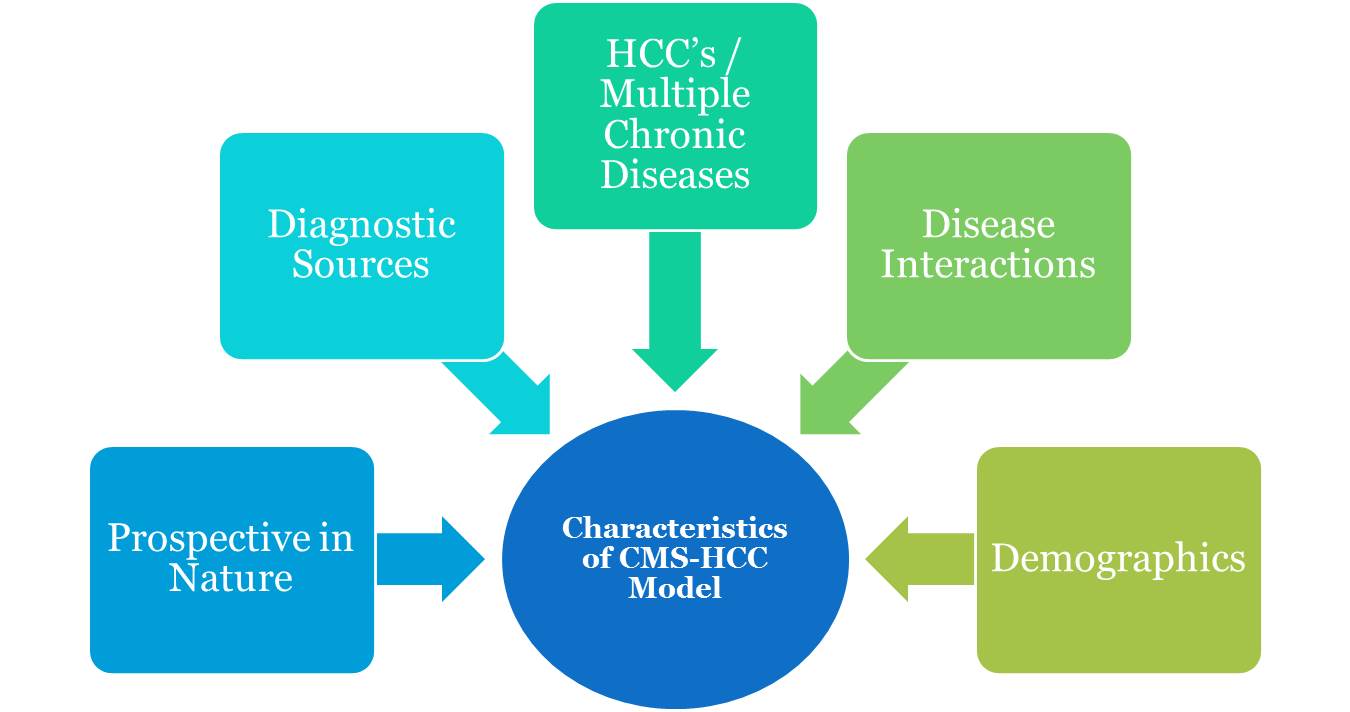
Characteristics of CMS HCC Model
Risk Adjustment 101
- Payment methodology used by Medicare Advantage health plan to adjust health plan payments
- Based on the enrollee health status and demographic characteristics
- Hierarchical Condition Category (HCC) Model
CMS HCC Model Principles
Principle 1: Diagnostic categories should be clinically meaningful.
Principle 2: Diagnostic categories should predict medical expenditures.
Principle 3: Diagnostic categories that will affect payments should have adequate sample sizes to permit accurate and stable estimates of expenditures.
Principle 4: Hierarchies are used to characterize the person’s illness level within each disease process, while the effect of unrelated disease processes increase predicted costs of care.
Principle 5: The diagnostic classification should encourage specific coding.
Principle 6: The diagnostic classification should not reward coding proliferation. The classification should not measure great disease burden simply because more diagnosis codes are present.
Principle 7: Providers should not be penalized for recording additional diagnoses. This principle has two consequences for modeling: (1) no condition category should carry a negative payment weight and,
(2) a condition that is higher-ranked in a disease hierarchy should have at least as large a payment weight as lower-ranked conditions in the same hierarchy.
Principle 8: The classification system should be internally consistent.
Principle 9: The diagnostic classification should assign all diagnosis codes.
Principle 10: Discretionary diagnostic categories should be excluded from payment models.
Reference:
